Top Boston doctors are worried about equal access to care in Massachusetts now that the U.S. decided to stop giving out free COVID vaccines as early as this fall.
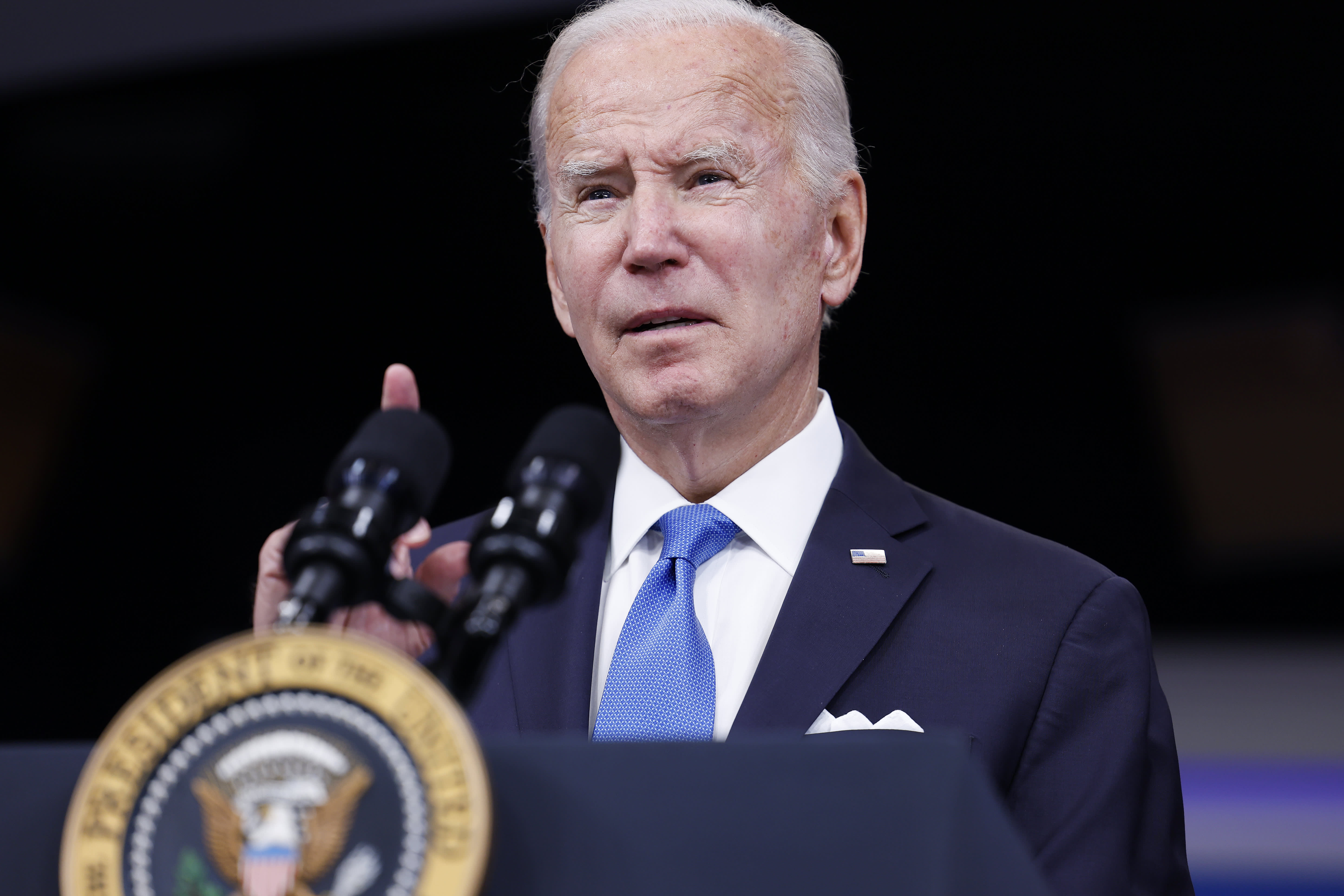
Shifting vaccine distribution to the private market is part of President Joe Biden's decision to end the national emergency and public health emergency declarations related to the pandemic in May. Some experts are concerned about shifting the cost to U.S. insurers and uninsured Americans who stand to lose access to vaccines.
WATCH ANYTIME FOR FREE
Stream NBC10 Boston news for free, 24/7, wherever you are. |
Tufts Medical Center's Dr. Shira Doron, Brigham and Women's Hospital's Dr. Daniel Kuritzkes and Boston Medical Center's Dr. Benjamin Linas discussed their concerns around health care access and equity in Massachusetts moving forward during NBC10 Boston's weekly "COVID Q&A" series.
"It's incredibly disappointing and depressing," Linas said. "Clearly the emergency situation at some level needs to be temporary -- it can't go forever. But we've learned so much in the last two years about some progress into potentially how we can find more equity in the way we deliver our health care. And we're just willfully going to tear that up at the eleventh hour."
Get updates on what's happening in Boston to your inbox. Sign up for our News Headlines newsletter.
The pandemic highlighted systemic inequities within the health care system, Linas said. The awareness helped inform the response to prioritize access in Massachusetts, thereby reducing the racial gap in vaccination rates. But the end of the emergency status not only means no more free vaccines, it also unravels other types of government support, according to Brigham and Women's chief of infectious disease.
"It's not just vaccine purchases that are going to end, everything is going to end," Kuritzkes said. "The government will no longer be providing test kits for free. The government will no longer be paying for antiviral treatment for people whether that's, you know, Paxlovid or other therapy. And so that is one of the reasons why the emergency declaration remained in place."
It's not just vaccine purchases that are going to end, everything is going to end.
Dr. Daniel Kuritzkes, Chief of Infectious Disease at Brigham and Women's Hospital
The biggest concern among top Boston doctors is that those structural barriers will return and people will fall through the cracks, particularly in communities of color, which are historically underrepresented and underserved when it comes to health care.
"I hope that part of the strategy of announcing that the end of the public health emergency is months away is going to be to use that time wisely to fill some of these gaps," Doron said. "I also think that this is an opportunity to look at how we might apply some of these lessons and how we might reach some of these gaps outside of COVID-19."
The U.S. has purchased vaccines directly from Pfizer and Moderna at an average price of about $21 per dose for the last two years, according to the Kaiser Family Foundation. The federal government has required pharmacies, doctor’s offices and hospitals to give out shots for free, regardless of insurance status. But that's all about to change.
"I don't think we have to postulate or expect or worry about what it will look like. We know what it will look like. It'll look like what things looked like before COVID, which means huge health care disparities, large gaps, especially in vaccine-preventable illnesses," Linas said.
The costs of COVID-19 vaccines are expected to skyrocket once the government stops buying them, with Pfizer saying it will charge as much as $130 per dose. Local experts say people should take advantage of the free updated booster while they still can.
"If you haven't been boosted in more than six months or longer, then you should definitely go ahead and get boosted. Now while it's still available to you," Kuritzkes said. "We don't know when the next round of boosters are going to be available. Presumably not until next fall."
Get updates on what's happening in Boston to your inbox. Sign up for our News Headlines newsletter.
The U.S. still has a substantial stockpile of free vaccines left, but it's unclear how long the supply will last. When the federal government stops buying COVID-19 vaccines, testing kits and drugs at a discount for the entire country, those who are uninsured could have to pay the full cost out of pocket.
"We have no idea what these tests are going to cost once they go on to the open market and are no longer being subsidized by the federal government, just as we have no idea what Paxlovid is going to cost and, you know, it snowballs from there," Kuritzkes said.
Local experts don't necessarily expect cases to go up as a result, but they do worry that the more vulnerable population will suffer once free testing kits are no longer available.
"People who are high-risk for progression to severe disease need to know they have COVID so that they can get early treatment. And the data show that treatment is really most effective -- or perhaps exclusively effective -- when given within five to seven days of illness depending on the drug," Doron said. "They won't have access to treatment, or know they need treatment, and they will suffer worse outcomes."